


-
-
Scientific LibraryAcute Coronary Syndrom ASCVD Prevention Bifurcation Stenting Cardio-Oncology Congestive Heart Failure DAPT Duration Drug Coated Balloon Fractional Flow ReserveNewsCases VideosE-LearningIndustry Insights
- LIVE
-
 Article Link
Article Link

The 6th World Symposium on PH: Hemodynamic Definitions and Updated Clinical Classification of PH
Saurabh Rajpal, Steven Stroud, Sophia Elizabeth Airhart, Veronica Franco, Riaz Rahman, Manreet Kanwar, Sasha Prisco, Kurt Prins
The 6th World Symposium on Pulmonary Hypertension proposed some fundamental changes to the hemodynamic and clinical classification of pulmonary hypertension (PH). We have summarized these changes below.
Change in Criteria for Diagnosis of PH - Based on the mean pulmonary artery pressure (mPAP) of 20 mmHg being 2 standard deviations above the mean value of 14.0 ± 3.3 mmHg, which was the normal value of mPAP observed in recent published data, and the fact that there have been multiple studies across different clinical types of PH documenting poor outcomes in patients with mPAP between 20 and 25 mmHg, it was proposed to define PH as mPAP >20 mmHg instead of mPAP ≥25 mmHg at rest, measured by right heart catheterization.
Pulmonary Vascular Resistance (PVR) Added to Definition of all Forms of Pre-Capillary PH - To identify pre-capillary PH as representative of pulmonary vascular disease, it was proposed to include PVR of ≥3 Wood units in the definition of all forms of pre-capillary PH associated with mPAP >20 mmHg.
Combined Pre- and Post-Capillary PH - The cutoff of ≥3 Wood units was also proposed to identify the group of patients that has combined pre- and post-capillary PH in addition to the mandatory pulmonary capillary wedge pressure of >15 mmHg and mPAP >20 mmHg, which is a prerequisite to be classified as having any type of post-capillary PH. This group of patients has worse prognosis compared with other patients with post-capillary PH.
Exercise PH - A definition for exercise PH could not reintroduced. The challenges of getting accurate right heart catheterization measurements and the lack of diagnostic discrimination power whether exercise PH is due to elevated pulmonary capillary wedge pressure (left heart disease) or pulmonary vascular disease makes it difficult to define exercise PH as an entity.
Drug- or Toxin-Associated PH - Drugs and toxins were divided into those with definitive association (epidemiologic outbreaks, case control and randomized control trials; e.g., dasatinib and methamphetamines) and those with possible association (e.g., cocaine).
Pulmonary Arterial Hypertension Long-Term Responders to Calcium Channel Blockers - These patients were introduced as a distinct group within Group I because they have been shown to have significantly better prognosis, unique management, and different pathophysiology. These patients are defined by a reactive vasodilators stress (a reduction of mPAP ≥10 mmHg to reach an absolute value of mPAP ≤40 mmHg with an increased or unchanged cardiac output) and a sustained hemodynamic response a year after being on calcium channel blockers and New York Heart Association Functional Class I/II.
Pulmonary Veno-occlusive Disease/Pulmonary Capillary Hemangiomatosis - These were defined as pulmonary arterial hypertension with overt features of venous/capillaries involvement was included in World Health Organization (WHO) Group I because their clinical presentation and hemodynamic profile are similar to PH.
WHO Group 4 Updates: PH due to Pulmonary Artery Obstructions - In addition to chronic thromboembolic PH, the entities included in this group were expanded to include other etiologies of pulmonary artery obstruction such as congenital pulmonary artery stenosis (Alagille syndrome) and malignant and non-malignant tumors.
WHO Group 5 Simplified - In the WHO Group 5 group, splenectomy and thyroid disease was removed as a subgroup and is considered as more of a risk factor for PH. Lymphangioleiomyomatosis was reclassified as WHO Group 3 because almost all cases of PH in lymphangioleiomyomatosis are associated with only mild PH but severe pulmonary parenchymal disease.
Table 1: Updated Hemodynamic Definition of PH
PH in Left Heart Disease
Pulmonary hypertension (PH) due to left heart disease is a complex condition encompassing different clinical phenotypes, pathophysiology, and prognoses. In an effort to clarify the disease process and provide clinical guidance, Vachiéry et al. propose a simplified phenotypic and hemodynamic approach in light of recent literature findings.
PH due to left heart disease is defined as elevated pulmonary pressure in response to elevated left atrial pressure. Elevated left-sided pressures can result from different pathologies, but generally speaking, left heart disease comprises three groups:
- 1. Heart failure with reduced ejection fraction
- 2. Heart failure with preserved ejection fraction (HFpEF)
- 3. Valvular heart disease
Among these subsets, PH can exist as the following:
- 1. Isolated post-capillary PH: Pulmonary artery wedge pressure (PAWP) >15 mmHg and mean pulmonary artery pressure (mPAP) >20 mmHg and pulmonary vascular resistance (PVR) <3 Wood units
- 2. Combined pre- and post-capillary PH: PAWP >15 mmHg and mPAP >20 mmHg and PVR ≥3 Wood units
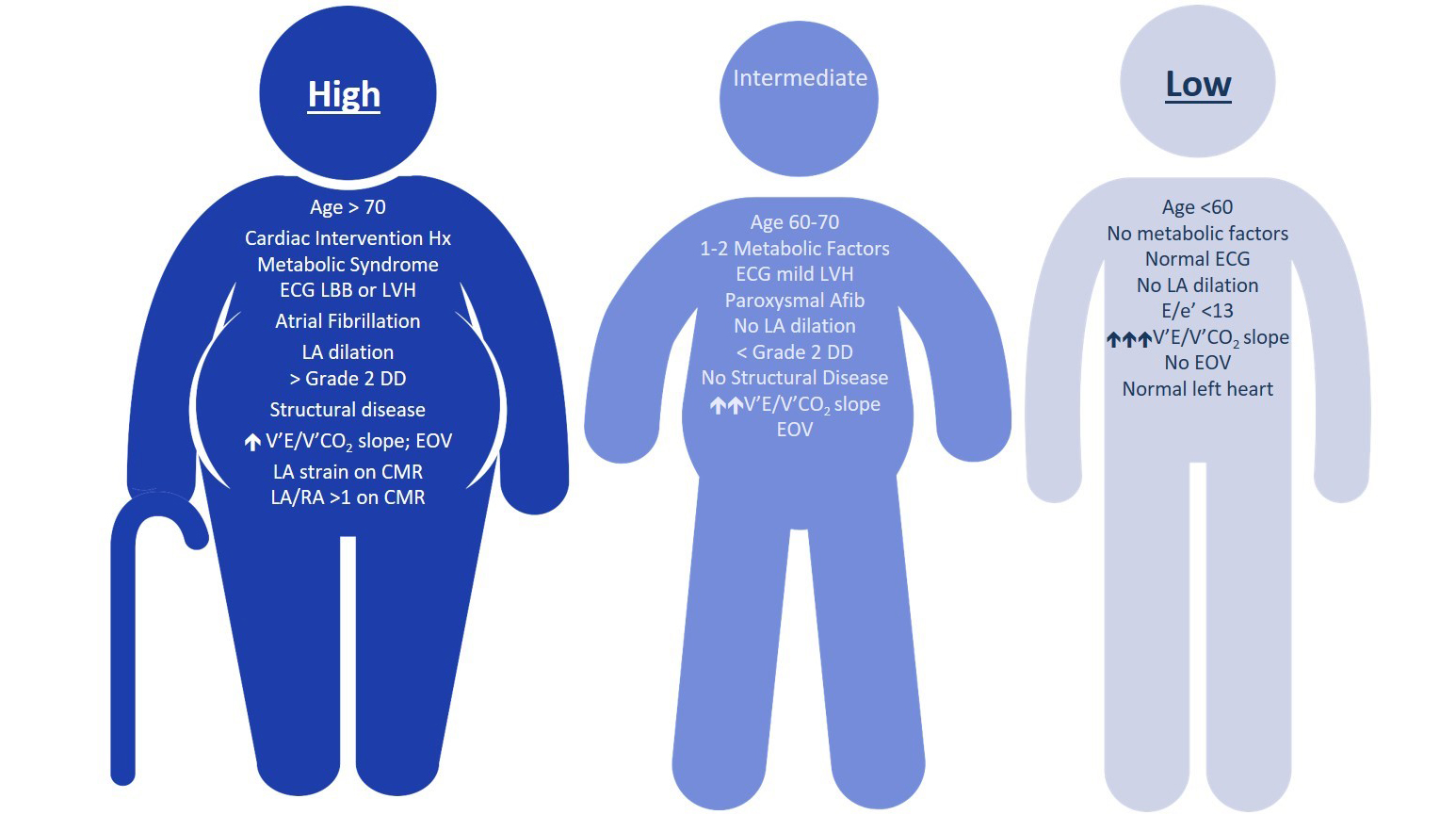
Consistent acquisition of key components during invasive hemodynamic testing with right heart catheterization remains challenging. Also, there is considerable difficulty delineating PH due to left heart disease from pulmonary arterial hypertension (PAH) with HFpEF because PAH patients often have concurrent cardiovascular disease. As such, the authors propose a three-phenotype classification system to refine PH due to left heart disease pre-test probability and stratify which patients require additional invasive studies (Figure 1):
- 1. High probability of left heart disease as a cause of PH. The general management should be guided according to the recommendation for the underlying condition.
- 2. Intermediate probability of left heart disease as a cause of PH. Invasive characterization may be performed in patients with risk factors for PAH (e.g., systemic sclerosis), chronic thromboembolic PH, or in cases of unexplained dyspnea. The presence of right ventricular abnormalities also requires invasive assessment because it may influence management.
Figure 1: Pre-Test Probability of PH due to Left Heart Disease Based on Clinical Phenotype
Resting Hemodynamic Evaluation of PH due to Left Heart Disease - If a patient exhibits an appropriate phenotype to warrant invasive hemodynamic studies, the following are proposed:
- 1. Right heart catheterizations should be performed in stable, non-critically ill patients and should be performed using proper leveling techniques, namely leveling at the mid-chest and "zero"ing the transducer to atmospheric pressure. Patients should be positioned supine with legs flat and pressures recorded during spontaneous breathing (no breath-hold).
- 2. Measure PAWP at end expiration and during end diastole (i.e., typically as the mean of the a-wave) for accurate assessment of PVR with special consideration during atrial fibrillation (when it is appropriate to measure PAWP 130-160 ms after the onset of QRS and before the V-wave).
- 3. Large V-waves should be reported because this strongly suggests left heart disease regardless of resting PAWP.
- 4. If there are discrepancies or ongoing diagnostic uncertainty, provocative testing with exercise testing or fluid challenge to elucidate the diagnosis is useful, particularly to distinguish between healthy subjects and HFpEF or to uncover PH due to left heart disease in patients with PAWP at the upper limit of normal (ULN) (i.e., 13-15 mmHg).
Provocative Hemodynamics - In patients with resting PAWP 13-15 mmHg and high/intermediate probability of PH with HFpEF, provocative testing should be considered to uncover PH due to HFpEF:
- 1. For technical reasons and reliability of pressure recording, a fluid challenge is preferred over exercise in the approach to differential diagnosis.
- 2. An increase of PAWP >18 mmHg after fluid loading in patients with resting values between 13 and 15 mmHg and intermediate/high probability of HFpEF may be considered abnormal.
- 3. The ULN of mPAP during an incremental dynamic exercise challenge has been suggested at >30 mmHg with a cardiac output (CO) <10 L•min−1, which corresponds to a total PVR (total peripheral resistance = mPAP/CO) of 3 Wood units.
- 4. The ULN of PAWP during exercise is thought to be between 15 and 25 mmHg, but higher values can be recorded in elderly subjects. A cut-off value of 25 mmHg is suggested for the diagnosis of heart failure, although PAWP >25 mmHg has been found in elderly individuals free of apparent cardiovascular disease.
- 5. A flow-adjusted measure of PAWP may be more appropriate than PAWP (i.e., PAWP/CO).
Calculations
- Diastolic pressure gradient = diastolic pulmonary artery pressure – Wedge pressure
- Transpulmonary pressure gradient (TPG) = mPAP – Wedge pressure
- PVR = (mPAP – Wedge pressure) / CO
- Pulmonary arterial compliance = stroke volume / (systolic pulmonary artery pressure – diastolic pulmonary artery pressure)
- Pulmonary artery elastance = systolic pulmonary artery pressure / stroke volume
Prognostic Factors
- ↑ Pulmonary artery elastance and ↓ pulmonary arterial compliance associated with worse prognosis
- ↑ TPG, PVR, and diastolic pressure gradient associated with worse outcomes
- ↑ PAWP/CO slope (>2 mmHg•L−1•min−1 is associated with reduced functional capacity, higher N-terminal pro-brain natriuretic peptide, and reduced heart failure-free survival)
Treatment of PH due to Left Heart Disease
- Mainstay of treatment is optimization of underlying left heart disease.
- No PAH therapies have been shown to be beneficial and may even lead to worse outcomes, specifically sildenafil in valvular heart disease post-intervention patients and macitentan in combined pre- and post-capillary PH.
PH in Patients With End-Stage Heart Failure
- Presence of PH signals poor prognosis after transplant. In the context of heart transplantation, PH is associated with an increased 30-day mortality in patients with TPG >15 mmHg and PVR >5 Wood units. Risk of morbidity and mortality increases with progressive elevation in mPAP, TPG, and PVR.
- It is recommended to perform right heart catheterization in all candidates before listing and at 3- to 6-month intervals in listed patients, especially in the presence of reversible PH or worsening heart failure.
- Acute vasodilator testing should be performed if systolic pulmonary artery pressure >50 and TPG ≥15 or PVR >3 Wood units.
- Left ventricular unloading with left ventricular assist device rapidly reverses PH due to left heart disease. Left ventricular assist device recipients with at least one post-implant right heart catheterization without PH likely require less frequent assessments.
Risk Stratification and Medical Treatment in PH
- 1. The progress observed in medical therapy of pulmonary arterial hypertension (PAH) over the last decade is not related to the discovery of new pathways but to the development of new strategies for combination therapy and on escalation of treatments based on systematic assessment of clinical response.
- 2. The current treatment strategy is based on the severity of PAH as assessed by a multiparametric risk stratification approach. Goals of therapy and factors associated with better prognosis include functional capacity Class I-II, 6-minute walk distance >400 meters, and normal right ventricular function per echocardiography and hemodynamic parameters.
- 3. Current treatment recommendations call for upfront oral combination therapy for low- and intermediate-risk patients with PAH and upfront combination therapy that should include parenteral prostacyclin therapy for patients with high-risk features.
- 4. Patients should be re-evaluated 3-6 months from the start of combination therapy. If goals of therapy are not met, sequential triple therapy or escalation of therapy from oral to parenteral prostacyclin is to be considered. Current recommendations are for evaluations every 3-6 months, particularly for the high-risk patients who may need lung transplant referral if they are refractory to maximal medical therapy.
- 5. Regarding vasoreactivity testing, it is recommended to evaluate response to calcium channel blockers only for patients with idiopathic PAH, heritable PAH, and PAH associated with drugs and toxins. If positive, very high doses of calcium channel blockers should be used (i.e., amlodipine 20 or 30 mg daily). If goals of therapy not achieved after 3-6 months, it is recommended to start specific PAH therapy.
- 6. Supportive therapy should include supervised exercise training.
- 7. Anticoagulation is not recommended for associated PAH but may be considered for idiopathic, heritable, or drug-induced PAH because data in those groups are less controversial.
- 8. Occasionally, patients have an extraordinary response to therapy, and transition to a less-invasive therapy is considered. Because much of the literature on this topic is retrospective, prospective but observational, or prospective randomised but open label, this approach is not recommended except in rare circumstances and under close expert care. There have been conflicting outcomes in the transition from parenteral prostacyclins to inhaled or oral prostacyclins. When discontinuation of bosentan is necessary due to liver function test elevations, transitioning to ambrisentan or macitentan is safe. At the time of the 6th World Symposium of PH, there was insufficient evidence to recommend transition from sildenafil or tadalafil to riociguat for improving efficacy, although studies are underway.
Chronic Thromboembolic PH
Chronic thromboembolic pulmonary hypertension (CTEPH) (World Health Organization Group 4) is defined as follows:
- - Hemodynamic findings of mean pulmonary artery pressure ≥25 mmHg, pulmonary artery wedge pressure ≤15 mmHg, and pulmonary vascular resistance ≥3 Wood units
- - In the presence of chronic, organized thrombi or emboli in the pulmonary arteries that persist despite at least 3 months of effective anticoagulation
The precise pathogenesis of CTEPH remains unclear but appears to be incited by acute pulmonary embolism with resultant altered vascular remodeling and endothelial dysfunction in the pulmonary arterial system. Chronic thromboembolic disease is characterized by similar symptoms and perfusion defects but without pulmonary hypertension at rest. CTEPH is an underdiagnosed condition that often presents with non-specific symptoms and requires a high index of clinical suspicion. Lung ventilation/perfusion scintigraphy is the screening test of choice; however, this test is infrequently ordered despite guideline recommendations.
Diagnosis is made by the following:
- History revealing signs and symptoms suggestive of CTEPH.
- Transthoracic echocardiography revealing evidence of pulmonary hypertension.
- VQ scan is the initial imaging test of choice. It has a high sensitivity and specificity. If there is no evidence of mismatched perfusion defect, CTEPH is effectively excluded.
- Computed tomography pulmonary angiogram then confirms diagnosis and assesses operability.
- Right heart catheterization and digital subtraction angiography are used to obtain invasive hemodynamics and determine accessibility of thrombi.
Treatment
- - Lifelong anticoagulation therapy.
- - Definitive therapy should be made by an expert CTEPH team.
- - Operable with acceptable risk/benefit: pulmonary thromboendarterectomy (treatment of choice).
- - Non-operable or operable with unacceptable risk/benefit: Targeted medical therapy and/or balloon pulmonary angioplasty (BPA).
- - Persistent/recurrent symptomatic pulmonary hypertension: consider re-do surgery versus targeted medical therapy and/or BPA.
- - Riociguat is approved for inoperable CTEPH (CHEST [A Study to Evaluate Efficacy and Safety of Oral BAY63-2521 in Patients With CTEPH]).
- - Macitentan also showed benefit for inoperable CTEPH (MERIT-1 [Clinical Study to Assess the Efficacy, Safety and Tolerability of Macitentan in Subjects With Inoperable Chronic Thromboembolic Pulmonary Hypertension]).
- - Unclear benefit of medical therapy as a bridge to pulmonary thromboendarterectomy surgery or as a bridge to BPA. Combining endarterectomy with BPA either as a hybrid or stepwise approach is being evaluated at select expert programs.
Summary - Pulmonary endarterectomy remains the treatment of choice for operable CTEPH. For those deemed inoperable, the best level of evidence supports initiation of medical therapy and consideration for BPA.
Figure 1: CTEPH Revised Treatment Algorithm

PH in Chronic Lung Disease and Hypoxia
Chronic lung disease-associated pulmonary hypertension (PH) is associated with reduced functional ability, impaired quality of life, greater oxygen requirements, and increased risk of mortality compared with patients with chronic lung disease. At this time, it is uncertain whether the presence of PH is causative or a surrogate of worse outcomes in chronic lung disease. However, patients with chronic lung disease-associated PH have the worst outcomes of all patients with PH.
Screening for PH in Chronic Lung Disease - Elevated plasma levels of brain natriuretic peptide and N-terminal pro-brain natriuretic peptide may increase suspicion for PH. Echocardiography is the best noninvasive modality to screen for chronic lung disease-associated PH. Ratio of main pulmonary artery to ascending aorta >1 may also predict PH.
Diagnosis - Right heart catherization is the gold standard for diagnosis of chronic lung disease-associated PH, but suspicion for underlying PH does not mandate the completion of right heart catherization, especially if the right heart catherization results will not influence therapy or management decisions, including referral for transplantation. Right heart catherization may be considered when clinical worsening, progressive exercise limitation and/or gas exchange abnormalities are not deemed attributable to ventilatory impairment and an accurate prognostic assessment is considered important. There are no valid data to support the routine use of acute vasodilator testing in chronic lung disease-associated PH.
Hemodynamic Definition - Chronic lung disease with PH is defined as mean pulmonary arterial pressure (mPAP) = 21-24 mmHg with pulmonary vascular resistance ≥3 Wood units or mPAP = 25-34 mmHg. Chronic lung disease with severe PH is defined as mPAP ≥35 mmHg or mPAP ≥25 mmHg with low cardiac index (<2.0 L•min−1•m−2).
Treatment - Currently, there are no strong data proving pulmonary arterial hypertension-specific therapy improves outcomes in chronic lung disease-associated PH. It is recommended that these patients be referred to expert centers for further treatment options.

http://www.cbsmd.cn Contact us by cbs@cbsmd.cn
Copyright ⓒ CBSMD Nanjing China. All rights reserved.



