CBS2017 CALENDAR
Event Highlights
Stenting Left Main
One or two stents for the distal Left Main bifurcation The DK crush V study - The DK crush V study
Tanveer Rab, MD, FACC ; Shao-Liang Chen, MD, FACC
Keywords: Transcatheter Cardiovascular Therapeutics, TCT17, Drug-Eluting Stents, Coronary Artery Disease, Tomography, Optical Coherence, Constriction, Pathologic, Confidence Intervals, Dilatation, Angioplasty, Balloon, Coronary, Percutaneous Coronary Intervention, Angina, Unstable, Stents, Coronary Artery Bypass, Myocardial Infarction, Thrombosis, Diabetes Mellitus, Algorithms
The DK (double kiss) CRUSH V trial reported at TCT2017 and published in the Journal of the American College of Cardiology(1) compared outcomes of a one stent provisional side branch(SB) stenting (PS) approach to the two stent (double kissing[DK]) crush technique for the distal Left Main true bifurcation (LMB).The primary endpoint was 1-year target lesion failure (TLF).
Two hundred and forty patients were randomized to DK and two hundred forty-two in the PS strategy. Baseline characteristics were well matched and diabetes was present in 27.2% of patients. Seventy percent of patients presented with unstable angina. The mean SYNTAX score was 30.6. Multivessel disease presented in 88.2% of patients. Medina class was 1,1,1 in 81.7 % and 0,1,1 in 18.3% of cases respectively.
Clinical follow up was obtained in all patients at one year and angiographic follow up at 13 months in 158 patients (65.3%) in the PS group and 159 patients (66.3%) in the DK group.
At one year, mortality was low at 1.2 % in the DK vs. 2.1 % in the PS arm (P=0.42). TLF occurred in 10.7% assigned to PS and 5.0% assigned to DK crush (HR 0.42, 95% CI 0.21-0.85, p=0.02). Compared to PS, DK crush also resulted in lower rates of target vessel myocardial infarction(TVMI) (2.9% vs. 0.4%, p=0.03) and definite or probable stent thrombosis (3.3% vs. 0.4%, p=0.02). Clinically-driven TLR (7.9% vs. 3.8%, p=0.06) and angiographic restenosis within the LM complex (14.6% vs. 7.1%, p=0.10) also tended to be less frequent with DK crush compared to PS. Rates of angiographic success and complete revascularization were similar in the two groups, although procedural time and contrast use were greater with DK crush stenting than PS.
An important aspect of the trial was outcomes of the two strategies based on lesion complexity (Figure 1). Involvement of the side branch (SB) determines lesion complexity. A simple lesion has a SB ostial stenosis of <70 % and lesion length <10 mm, whereas in a complex lesion SB ostial stenosis is ≥70 % with a lesion length ≥10 mm. Added criteria for increasing lesion complexity based on the DEFINITION(2) study were any 2/6 minor criteria (distal bifurcation angle <450 or ≥700, MV reference vessel diameter ≤2.5 mm, MV lesion length ≥25 mm, multiple bifurcations, thrombus-containing lesion, and severe calcification).
SB pre-dilatation was performed in 39.7% of patients in PS group due to severe SB compromise after MV treatment. A total of 114 (47.1%) patients in PS group required an additional SB stent for suboptimal results after MV stenting, including 64/165 (38.8%) patients with simple LM bifurcation lesions and 50/77 (64.9%) patients with complex lesions (p=0.001). A SB stent was successfully implanted in all DK crush patients. The proximal optimization technique (POT) and final kissing balloon inflation (KBI) were more frequently used in the DK crush group than the PS group. In the 114 patients in the PS group who required a SB stent vs. the 128 patients who did not, the 1-year rates of TLF were 13.2% vs. 8.6% respectively (p=0.30), and the 1-year rates of ST were 6.1% vs. 0.8% respectively. Angiographic restenosis primarily at the left circumflex ostium occurred in 14.6% patients treated with PS vs. 7.1% patients treated with DK crush (p=0.10). Interestingly, left circumflex ostial restenosis was similar at 12% with a single stent provisional approach in the EXCEL(3) and NOBLE(4) trials.
As demonstrated in the central illustration (Figure 1), in a simple LMB there were comparable outcomes with a single stent PS with a I- year TLF of 8.3 % vs 5.0 % with DK techniques (p=0.45). With a more complex LMB lesion TLF was 18.0% with PS and 4.8% with DK (p=0.018).
Results of the DK CRUSH V trial support our treatment algorithm(5) for LMB stenting strategies (Figure 2). A suggested approach to LM intervention is to first assess whether the lesion is simple or complex (Figure 1) and then proceed with a stenting approach as described in the algorithm.
Legends
TLF: Target Lesion failure
Click on Figure 1 to view a full size version.

ABC = Asian Bifurcation Club; DK = double kiss; EBC = European Bifurcation Club; FFR = fractional flow reserve; IVUS = intravascular ultrasound; LM = left main coronary artery; OCT = optical coherence tomography; SB = side branch (generally the left circumflex); TIMI = Thrombolysis In Myocardial Infarction; T/TAP = T-stenting or T-stenting and minimal protrusion.
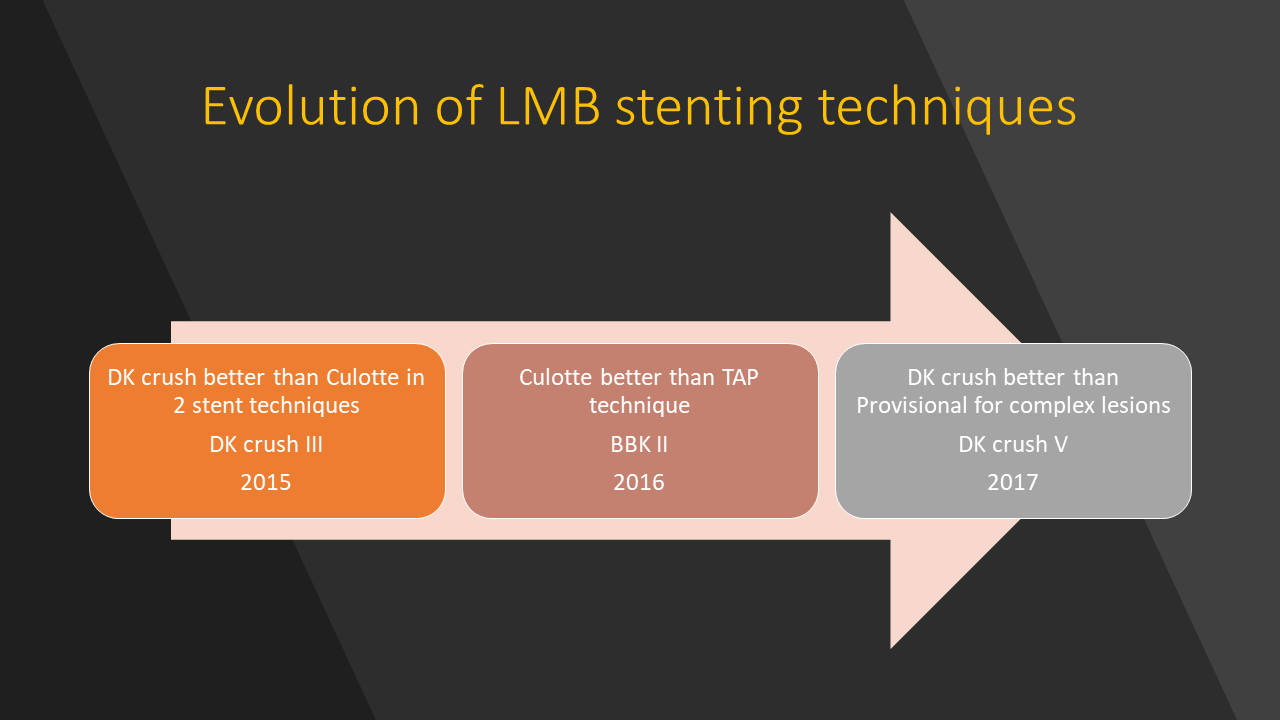
Figure 3 Evolution of Left Main Bifurcation trials
DK crush V(1)