推荐文献
Original Research2017 Nov 14;70(20):2476-2486.
JOURNAL:J Am Coll Cardiol. Article Link
Shah KS, Xu H, Fonarow GC et al. Keywords: ejection fraction; heart failure; outcomes; survival
BACKGROUND - Patients with heart failure (HF) have a poor prognosis and are categorized by ejection fraction (EF).
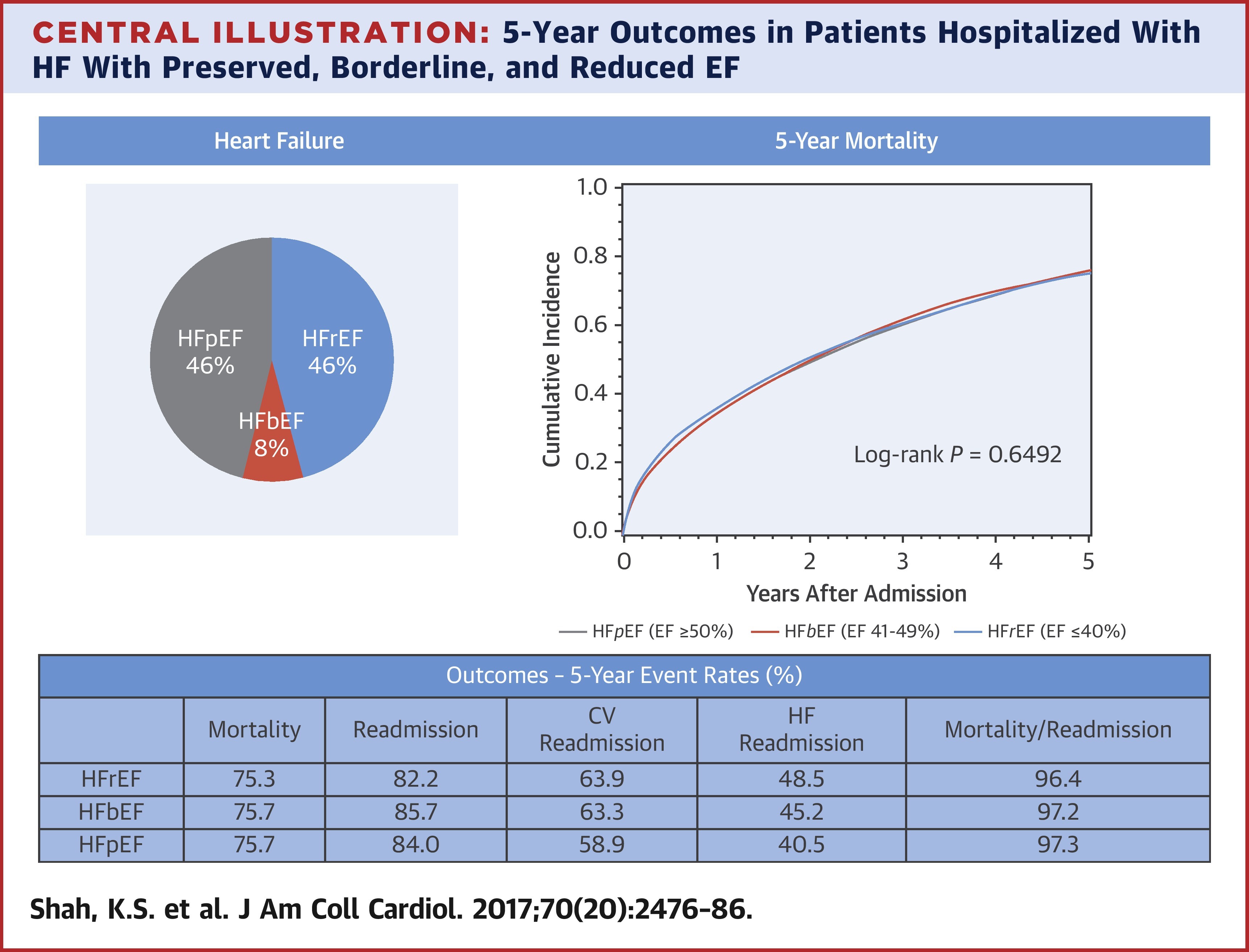
OBJECTIVES - This study sought to characterize differences in outcomes in patients hospitalized with heart failure with preserved ejection fraction (HFpEF) (EF ≥50%), heart failure with borderline ejection fraction (HFbEF) (EF 41% to 49%), and heart failure with reduced ejection fraction (HFrEF) (EF ≤40%).
METHODS - Data from GWTG-HF (Get With The Guidelines-Heart Failure) were linked to Medicare data for longitudinal follow-up. Multivariable models were constructed to examine 5-year outcomes and to compare survival to median survival of the U.S. population.
RESULTS - A total of 39,982 patients from 254 hospitals who were admitted for HF between 2005 and 2009 were included: 18,299 (46%) had HFpEF, 3,285 (8.2%) had HFbEF, and 18,398 (46%) had HFrEF. Overall, median survival was 2.1 years. In risk-adjusted survival analysis, all 3 groups had similar 5-year mortality (HFrEF 75.3% vs. HFpEF 75.7%; hazard ratio: 0.99 [95% confidence interval: 0.958 to 1.022]; HFbEF 75.7% vs. HFpEF 75.7%; hazard ratio: 0.99 [95% confidence interval: 0.947 to 1.046]). In risk-adjusted analyses, the composite of mortality and rehospitalization was similar for all subgroups. Cardiovascular and HF readmission rates were higher in those with HFrEF and HFbEF compared with those with HFpEF. When compared with the U.S. population, HF patients across all age and EF groups had markedly lower median survival.
CONCLUSIONS - Among patients hospitalized with HF, patients across the EF spectrum have a similarly poor 5-year survival with an elevated risk for cardiovascular and HF admission. These findings underscore the need to improve treatment of patients with HF.
Copyright © 2017 American College of Cardiology Foundation. Published by Elsevier Inc. All rights reserved.